VALVE DEFECTS AND DIAGNOSIS
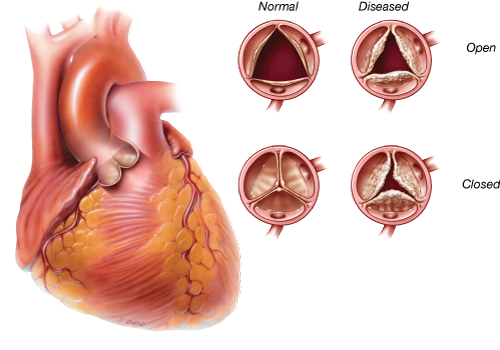
Heart valves can fail by becoming narrowed (stenotic) so that they block the flow of blood or leaky (regurgitant) so that blood flows backward in the heart. Sometimes a valve is both stenotic and regurgitant. A variety of conditions can cause these heart valve abnormalities.
Causes of Heart Valve Disease
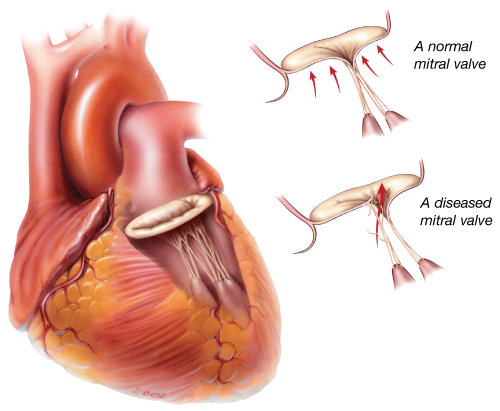
Degenerative valve disease:
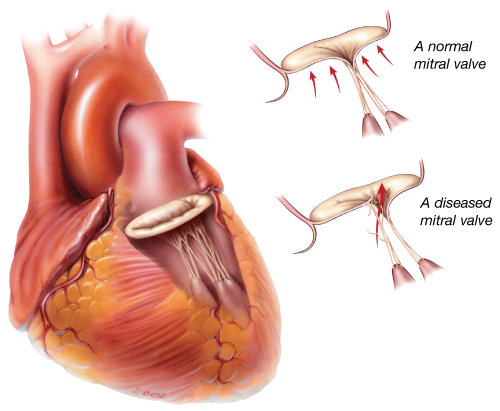
This is a common cause of valvular dysfunction. Most commonly affecting the mitral valve, it is a progressive process that represents slow degeneration from mitral valve prolapse (improper leaflet movement). Over time, the attachments of the valve thin out or rupture, and the leaflets become floppy and redundant. This leads to leakage through the valve.
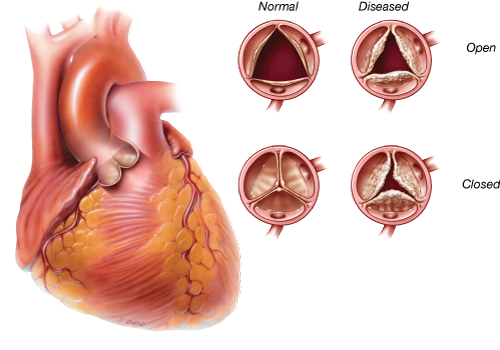
 Calcification due to aging
Calcification due to aging Calcification refers to the accumulation of calcium on the heart’s valves. The aortic valve is the most frequently affected. This build-up hardens and thickens the valve and can cause aortic stenosis, or narrowing of the aortic valve. As a result, the valve does not open completely, and blood flow is hindered. This blockage forces the heart to work harder and causes symptoms that include chest pain, reduced exercise capacity, shortness of breath and fainting spells. Calcification comes with age as calcium is deposited on the heart valve leaflets over the course of a lifetime. To learn more about aortic stenosis, please visit or
 Coronary artery disease
Coronary artery disease:
Damage to the heart muscle as a result of a heart attack can affect function of the mitral valve. The mitral valve is attached to the left ventricle. If the left ventricle becomes enlarged after a heart attack, it can stretch the mitral valve and cause the valve to leak.
Rheumatic fever:
Once a common cause of heart valve disease, rheumatic fever is now relatively rare in most developed countries. Rheumatic fever is caused by an infection of the Group A Streptococcus bacteria and can detrimentally affect the heart and cardiovascular system, especially the leaflet tissue of the valves. When rheumatic fever affects a heart valve, the valve may become stenotic, regurgitant or both. It is common for the heart valve abnormality to become apparent decades after the bout of rheumatic fever.
Congenital abnormalities:
Congenital heart defects (present at birth) can affect the flow of blood through the cardiovascular system. Blood can flow in the wrong direction, in abnormal patterns, and can even be blocked, partially or completely, depending on the type of heart defect present. Ranging from mild defects such as a malformed valve to more severe problems like an entirely absent heart valve, congenital heart abnormalities require specialized treatments.
Bacterial endocarditis:
Bacterial endocarditis is a bacterial infection that can affect the valves of the heart causing deformity and damage to the leaflets of the valve(s). This usually causes the valve to become regurgitant, or leaky, and is most commonly seen in the mitral valve.
Diagnosis of Valve Disease
Before a patient sees a primary care physician or a cardiologist (a doctor who specializes in understanding the heart) concerning a heart valve problem, he or she has often experienced some type of physical sign or discomfort. Some physical signs of heart valve disease include: angina (chest pain), tiredness, shortness of breath, lightheadedness or loss of consciousness.
However, in some cases a heart valve problem may cause no symptoms at all. These heart valve issues can often be identified by use of a stethoscope on routine physical examination. Heart valve abnormalities, whether stenosis or regurgitation, often produce a heart murmur. A heart murmur, particularly if it is new or loud, should prompt further investigation by your physician.
Cardiologists and surgeons have many ways of diagnosing heart valve disease. The most important is the echocardiogram.
Echocardiography
Echocardiography is a special application of ultrasound that enables the cardiologist to observe the function of your heart valves and the contractions of your heart muscle. During an echocardiogram, ultrasound waves are projected onto the heart. The reflected ultrasound is “captured” by a transducer, and a computer translates the sound waves into an image. Most echocardiograms are performed by placing the ultrasound probe on a person’s chest. This is called a “transthoracic” or “surface” echocardiogram. This test is non-invasive and takes only a few minutes.
In some cases, a tranesophageal echocardiogram is performed. With this type of echocardiogram, the ultrasound probe is inserted into the esophagus through the mouth. Because the esophagus is very close to the back of the heart, this sort of echocardiogram provides excellent images of the heart and its valves.
Catheterization
Cardiac catheterization (angiography) helps to determine the function of the coronary arteries and the heart valves. Cardiac catheterization is the process by which a tube is inserted into the blood vessels and/or heart. The tube injects a contrast medium (dye) which is then visualized with X-rays. Coronary angiography is particularly useful for analyzing the coronary vessels of the heart. Most patients have a coronary angiogram, or cardiac catheterization, before heart valve surgery; this is necessary to determine whether any blocked coronary arteries require treatment at the time of surgery.
Chest X-ray
A chest X-ray can be important in the detection of calcium deposits in the heart, such as on heart valves. It will also show the size and shape of the heart and lungs. All patients will have a chest X-ray before heart valve surgery.
VALVE TREATMENT
Diseased heart valves can be addressed in several ways. These include: 1) medication; 2) surgical valve repair; 3) surgical valve replacement; and 4) transcatheter valve replacement. While medication cannot correct valve dysfunction, it can alleviate symptoms in many cases. If repair or replacement becomes necessary, your cardiologist, surgeon or interventional cardiologist, will discuss the options with you. The choice between replacement or repair will depend on a number of factors, including the specific valve in question, the severity of the condition and whether the issue is stenosis or regurgitation.
Your Heart Team
If you will be undergoing a heart valve repair or replacement procedure, you will be cared for by a team of medical specialists who are committed to ensuring your safety and comfort before, during, and after, your procedure. Below you will find information describing different health care professionals you may meet during the course of your care.
Primary care physician:
May be the first to identify the symptoms of heart valve disease or conditions that can cause heart valve disease or defects. He or she may order special tests to confirm the diagnosis or refer you to the appropriate specialist.
Cardiologist:
A physician who specializes in diseases of the heart. The cardiologist does not perform heart surgery but often performs diagnostic studies to identify the cause of heart problems and determine the course of treatment to manage heart disease. The cardiologist may prescribe medications and/or refer you to a cardiovascular surgeon.
Cardiovascular surgeon:
A physician who specializes in heart surgery, including the repair or replacement of diseased heart valves. The surgeon will help in the decision making process about timing and best course of action, including approach and device choice for your valve disease.
Interventional cardiologist:
A physician who has additional specialized training to perform catheter-based procedures to treat heart diseases. The interventional cardiologist will work with the surgeon to determine the right candidates for transcatheter aortic valve replacements.
Anesthesiologist:
The anesthesiologist (doctor) or anesthetist (nurse) are trained to provide sedation or general anesthesia (sleep) during interventional procedures.
Critical care physicians and nurses:
The critical care or intensive care unit is a specialized area in a hospital where you are closely monitored and treated after most interventional procedures. Working with your surgeon and/or cardiologist, the critical care team physicians and nurses manage your care during this time.
Surgical Approaches for Heart Valve Disease
Most heart surgery is performed through an incision across the full length of the breast bone, or sternum. This incision is called a median sternotomy. It generally heals quite well, with the bone requiring about 6 weeks for complete healing.
In selected patients, heart valve surgery can be performed using smaller, or minimally invasive, incisions. Smaller incisions may provide some benefit to patients. Preoperative studies, including a coronary angiography, echocardiography and, in many cases, chest CT (CAT) scan, help to determine which patients are candidates for minimally invasive surgery. These surgical approaches with small incisions also include use of the heart lung machine as do full sternotomy operations.
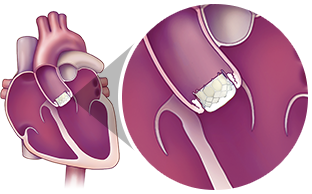
Transcatheter Aortic Valve Replacement (TAVR): A Less Invasive Option to Open Heart Surgery
For people who have been diagnosed with severe aortic stenosis and who are moderate or greater-risk for open heart surgery, another option is available—transcatheter aortic valve replacement (TAVR). This procedure can also be referred to as transcatheter aortic valve implantation (TAVI). It is a less invasive procedure that does not require open heart surgery.
The TAVR procedure allows a new valve to be inserted with your diseased aortic valve. The new valve will push the leaflets of your diseased valve aside. The frame will use the leaflets of your diseased valve to sure it in place.
This less invasive procedure is different than open heart surgery. TAVR uses a catheter to replace the heart valve instead of opening the chest and completely removing the diseased valve.
The TAVR procedure can be performed through multiple approaches, how the most common approach is the transfemoral approach (through an incision in the leg). Only a Heart Team can decide which approach is best, based on a person's medical condition and other factors.
Please consult a Heart Team for more information on TAVR and its associated risks
Surgical Valve Replacement
If the cardiovascular surgeon chooses to replace the patient’s heart valve, the first step is to remove the diseased valve (excise the valve and calcium deposits) and then implant a prosthetic heart valve in its place. Prosthetic valves used to replace diseased natural valves are made from a variety of materials and come in a variety of sizes.
There are two broad categories of prosthetic heart valves that are used to replace diseased valves:
- Bioprosthetic or tissue valves made primarily from animal tissue [i.e., bovine (cow) pericardium (the tough sac surrounding its heart), a porcine (pig) aortic valve, or human valves taken from cadavers]
- Mechanical valves constructed from synthetic material, primarily carbon
Tissue Valves (Bioprosthetic Valves)
There are a wide variety of tissue valves:
- Heterograft (or Xenograft) - valves or pericardial tissue harvested from medical-grade animals (i.e., bovine (cow) or porcine (pig))
- Homograft (or Allograft) - human valves taken from cadavers
- Autograft/Autologous tissue:
normal valve that has been transferred from one position to another replacing a diseased valve within the same individual (confined to a pulmonic valve used to replace an aortic valve).
A heterograft is a biological valve made from animal tissue. For example, pericardial valves traditionally contain leaflets made from bovine (cow) pericardium (the sac surrounding its heart) and are sewn onto a flexible or semi-flexible frame. Another type of tissue valve is a porcine valve. A porcine valve is made from pig’s aortic heart valve and is usually sewn onto a flexible or semiflexible frame to make a “stented” valve; alternatively, the natural porcine aortic root is left intact to function as the frame to make a “stentless” valve.
Each valve is surrounded by a cloth sewing ring. Sutures are placed through this sewing ring to secure the valve to the heart.

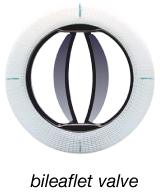
Mechanical Valves
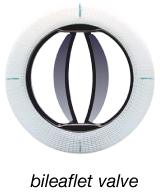
Mechanical valves include leaflets that are made out of a special type of carbon. These valves usually have two leaflets. The leaflets open and close during the cardiac cycle, ensuring flow of blood in one direction.
Criteria and Selection of Heart Valves
The choice between a mechanical and tissue valve depends upon an individual assessment of the benefits and risks of each valve and the lifestyle, age and medical condition of each patient.
Tissue valves do not require long-term use of blood thinners (anticoagulants). This is an important consideration for those who cannot take blood thinners because of a previous history of major bleeding (e.g., gastrointestinal or genitourinary) or an increased risk of traumatic injury and bleeding related to recreational activity, sports, or advanced age. Tissue valves generally last at least 10 years and, in some people, have lasted longer than 30 years. If a patient under 60 years of age receives a tissue valve, there is a high probability that he or she will require another valve replacement at some point; whereas, most patients who are 70 years and older do not.
Mechanical valves rarely wear out. However, they require daily treatment with blood thinners, and blood thinners can require changes in diet or activity levels.
The decision to choose a tissue or mechanical valve replacement is often related to the patient’s age, with older patients preferentially receiving tissue valves. However, there is no clear agreement on the precise age cutoff where a tissue valve may be preferable to a mechanical valve.
Valve Repair
When possible, it is generally preferable to repair a patient’s valve rather than to replace it with a prosthetic device. Valve repair usually involves the surgeon modifying the tissue or underlying structures of the mitral or tricuspid valves.
Nearly all valve repairs include placement of an annuloplasty ring or band. This is a cloth-covered device that is implanted around the circumference, or annulus, of the mitral or tricuspid valve. It provides support to the patient’s own valve and brings the valve leaflets closer together, potentially reducing leaks across the valve. There are a variety of different annuloplasty devices. The surgeon will choose one that best fits your heart valve.

In addition to an annuloplasty, mitral valve repair frequently requires correction of problems with the leaflets or chords, which attach the valve leaflets to the heart. When a mitral valve leaks because of mitral valve prolapse, fixing the leaflets and chords (and adding an annuloplasty ring or band) restores normal valve function.
Care After a Heart Valve Procedure
The normal recovery period from standard heart valve surgery requires four to eight weeks. Recovery may be faster when a smaller incision is employed, for example, with minimally invasive and transcatheter procedures. During this time, patients gradually gain energy and resume normal activities of daily living. Regular check-ups by a heart specialist are essential, and you are encouraged to call or see your doctor whenever you have questions or concerns about your health, especially if you experience any unusual symptoms or changes in your overall health.
Diet and Exercise:
Two additional important aspects of recovery and general wellness are maintenance of a healthful diet and regular exercise. If your doctor has recommended a special diet, it is important that it be followed. Healthy eating is an important part of a healthy life. During recovery, nutritious food gives your body energy and can help you heal more quickly.
To improve overall cardiovascular fitness, it is recommended that you combine a balanced diet with your doctor’s recommendations about exercise and weight control. Following a regular exercise program is an important part of maintaining a healthy lifestyle. Under your doctor’s guidance, you should gradually build up your exercise and activity level. Before you begin a new sports activity, check with your doctor.
Anticoagulants:
It is important to follow your doctor’s directions for taking medications, especially if an anticoagulant has been prescribed. Anticoagulants, or blood thinners, decrease the blood’s natural ability to clot. If you must take anticoagulant drugs, you will need periodic blood tests to measure the blood’s ability to clot. This test result helps your doctor determine the amount of anticoagulant you need. It may take a while to establish the right dosage of this drug for you, but consistency and working with your doctor are important. Home testing may also be available, so check with your physician about this option. Consult your doctor about interactions with any other drugs you may be taking and dietary restrictions you may have while taking anticoagulants, and also ask about any signs to watch for that might indicate your dosage is too high.
Other Health Information:
Before any dental work, including teeth cleaning, endoscopy or surgery is done, tell your dentist or doctor about your prosthetic heart valve. Patients with a valve implant are more susceptible to infections that could lead to future heart damage. Therefore, it may be necessary to take antibiotics before and after certain medical procedures to reduce the risk of infection.